Building a Resilient Nursing Workforce: Strategies for Sustainable Nurse Staffing
The nursing profession faces many challenges, including staff shortages and burnout, jeopardizing patient care and nurse well-being.
It’s only natural to seek solutions to these pressing issues.
This article offers a roadmap for resilience and sustainability in nurse staffing, ensuring you have the proper knowledge to tackle these issues in this industry.
We will cover:
The importance of building a resilient nursing workforce
5 key strategies for sustainable nurse staffing
Future trends that will define nurse staffing
Continue reading to uncover strategies that can transform challenges into opportunities for growth and resilience in nursing.
The Importance of Building a Resilient Nursing Workforce
Building a resilient nursing workforce is crucial for the healthcare sector because it helps face global health challenges and ensures patient care continuity and quality. Resilience in nursing encompasses the ability to adapt, recover, and grow in the face of stressors and challenges inherent in the healthcare environment. Given nursing work's high-stress, high-stakes nature, this capability is essential.
Let’s see some other advantages.
Firstly, resilience contributes to reducing burnout among nurses. Burnout, characterized by emotional exhaustion, depersonalization, and a diminished sense of personal accomplishment, significantly affects nurses' mental health and job satisfaction. A resilient workforce can better manage stress, maintain emotional stability, and sustain high job satisfaction and engagement. This, in turn, leads to lower turnover rates, reducing the costs and disruptions associated with recruiting and training new staff.
Moreover, resilient nurses are better equipped to deliver high-quality patient care. They can remain focused, make critical decisions under pressure, and maintain a compassionate approach despite the challenges. This ability directly impacts patient outcomes, satisfaction, and safety, reinforcing the essential role of resilience in clinical excellence.
Resilience also fosters a positive workplace culture. When nurses are resilient, they can support one another, create a more positive work environment, and effectively work as a team. This culture of resilience can lead to innovative problem-solving and improved efficiency within healthcare settings.
Finally, preparing for future healthcare challenges needs a resilient nursing workforce. The healthcare landscape is ever-evolving, with emerging diseases, technological advancements, and changing patient demographics. Resilient nurses can adapt to these changes, embrace new learning opportunities, and continue to provide effective care in an increasingly complex healthcare environment.
5 Key Strategies for Sustainable Nurse Staffing
We already discussed the advantages of building a resilient nursing workforce. That’s why Investing in resilience training and support systems for nurses is a strategic priority for healthcare organizations aiming for sustainability and excellence in care delivery.
Let’s see the practical strategies you can implement to build a resilient nursing workforce with actionable steps and examples.
1) Implement Flexible Staffing Models
Implementing flexible staffing models allows healthcare facilities to adapt to fluctuating patient care needs efficiently while also considering the well-being of the nursing staff. By embracing flexibility, you can ensure that staffing levels meet patient needs and are sustainable for nurses.
Here are some ways to leverage flexible staffing models:
Cross-Training Nurses: Invest in cross-training your nurses in various specialties. This enhances their skill sets and allows for more versatile staffing options. For example, a nurse trained in both pediatric and adult care can seamlessly support different units as patient demand shifts.
Implementing a Float Pool: Develop a pool of nurses who can work across multiple departments. This 'float pool' lets you dynamically allocate staff based on the most pressing needs. Ensure these nurses are rewarded for their flexibility with incentives such as higher pay rates or more control over their schedules.
Using Predictive Analytics: Employ predictive analytics to forecast patient admissions and peak periods. By analyzing trends and historical data, you can anticipate staffing needs and adjust schedules proactively rather than reactively.
Example Spotlight: Reading Hospital
Integrating predictive analytics allowed Reading Hospital to develop a staffing model that dynamically adjusted core and flexible staffing based on actual and anticipated needs. This model significantly reduced instances of over- and under-staffing by providing a clear depiction of staffing needs in real-time through a "heat map" visual aid. Managers and directors, initially hesitant about losing scheduling control, were convinced of the model's efficacy when they saw improvements in staffing balance.
2) Foster a Supportive Work Environment
A supportive work environment influences nurse retention because it can mitigate burnout, encourage professional growth, ensure nurses feel valued and understood, and stabilize staffing levels.
Here are a few tips for creating a more supportive work environment:
Establish Open Communication Channels: Promote an organizational culture where nurses feel comfortable voicing concerns and suggestions. Regularly scheduled feedback sessions can facilitate this, ensuring that nurses are heard and their input is valued.
Mentorship Programs: Implement mentorship programs where experienced nurses mentor newcomers. This not only aids in the professional development of new staff but also fosters a sense of belonging and community.
Recognition and Reward Systems: Develop systems to recognize and reward nurses for their hard work and dedication. Recognition can be as simple as a personal note of thanks or as significant as awards for exceptional service. These gestures show appreciation and can significantly boost morale.
Example Spotlight: Cleveland Clinic
The Cleveland Clinic's "Office of Nursing Research and Innovation" exemplifies how fostering a supportive work environment can lead to sustainable nurse staffing. The initiative encourages nurses to engage in research and innovation projects to improve patient care and nursing practices.
The clinic provides resources, funding, and mentorship, empowering nurses to pioneer solutions to the challenges they face in their daily work. This approach enhances the quality of patient care and significantly boosts job satisfaction and professional growth among nurses.
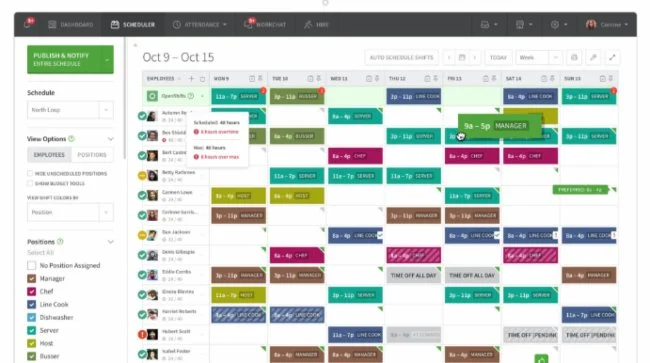
3) Use Advanced Scheduling Technology
Using advanced scheduling technology enhances efficiency and reduces nurses' administrative burden. By leveraging such technologies, healthcare facilities can match staffing levels with patient care needs in real time, anticipate staffing needs, and offer nurses more control over their schedules.
Here are some tips for using advanced scheduling technology:
Implement Predictive Analytics: Use predictive analytics tools to forecast staffing needs based on historical patient admission rates, seasonal trends, and other relevant factors. This approach allows for proactive rather than reactive scheduling, ensuring the right number of nurses are on duty at the right times.
Adopt Self-Scheduling Tools: Provide nurses with access to self-scheduling software. Empowering them to choose shifts that best fit their life and work balance increases job satisfaction and retention.
Use Mobile Applications: Implement mobile scheduling applications that allow nurses to view their schedules, swap shifts, and communicate with scheduling coordinators on the go. As such, you increase flexibility and responsiveness to staffing needs.
Example Spotlight: West Hospital VCU Health
The West Hospital VCU Health case study in the American Nurse Journal highlights implementing an electronic nurse scheduling system (ENSS) to enhance staffing efficiency, financial performance, and nurse satisfaction.
Adopting ENSS allowed the hospital to effectively predict, plan, and adjust staffing needs in real time, ensuring optimal patient care and nurse workload. The system also promoted staff involvement in scheduling, leading to increased fairness and accountability. This approach improved operational efficiency and nurse retention, underscoring the benefits of technology in healthcare staffing.
4) Focus on Retention through Professional Development
Focusing on retention through professional development leads to sustainable nurse staffing by enhancing engagement, promoting career progression, and improving patient care quality.
Here's how to leverage this strategy:
Offer Continuous Education Opportunities: Implement programs that allow nurses to acquire new skills and certifications relevant to their field and interests. As such, they can stay up-to-date with the latest practices and you can foster a culture of lifelong learning.
Create Leadership Development Pathways: Establish clear pathways for nurses to advance into leadership roles. Think mentorship programs, leadership training, and opportunities for shadowing current leaders.
Encourage Specialization: Support nurses in specializing in areas they are passionate about. You could consider funding for specialized training or allowing time off for education.
Example Spotlight: The American College of Cardiology
The American College of Cardiology offers a compelling example of enhancing nurse retention through professional development. We’re talking about the tertiary care hospital's cardiovascular (CV) intensive care unit (ICU).
They introduced a competency-based professional advancement program focused on clinical nursing education, unit-based competencies, and professional development.
This initiative reduced nursing attrition rates by 73%, demonstrating the positive impact of tailored professional development and education on nurse retention, even amidst increasing patient volume and acuity.
5) Adopt a Holistic Approach to Wellness and Resilience
Adopting a holistic approach to wellness and resilience is vital for sustainable nurse staffing. This strategy supports nurses' overall well-being, addressing their physical and mental health needs.
Obviously, health is crucial in a high-stress profession.
However, focusing on comprehensive wellness programs allows hospitals and healthcare facilities to enhance engagement and improve retention rates among nursing staff.
Here are some tips to get you started:
Implement Wellness Initiatives: Offer accessible resources for physical health, such as fitness programs, nutrition counseling, and health screenings. These initiatives can improve physical well-being, reduce absenteeism, and raise energy levels among nurses.
Promote Mental Health Support: Establish support systems for mental health, including stress management workshops, counseling services, and resilience training. These resources help nurses cope with the emotional demands of their roles, fostering a supportive work environment.
Ensure Work-Life Balance: Support flexible scheduling and provide resources for personal life management, such as childcare services and financial planning assistance. Encouraging a balance between professional and personal life can significantly enhance job satisfaction and loyalty.
Example Spotlight: Vanderbilt Nurse Wellness Program
The Nurse Wellness Program at Vanderbilt recognizes the pressures and stressors unique to the nursing profession, offering structured support to enhance their overall well-being and job satisfaction.
Addressing professional and personal challenges aims to foster a healthier work environment and support nurses in maintaining a balance between their work and personal lives, which is crucial for long-term retention.
The Future of Sustainable Nurse Staffing
The healthcare landscape is undergoing transformative changes, with emerging trends promising to reshape nursing profoundly. This section explores the implications of these shifts and outlines the anticipatory steps needed to navigate future challenges and opportunities.
Technological Integration and Nursing Evolution
Integrating technologies such as artificial intelligence (AI) and telehealth is redefining the boundaries of nursing practice. Nurses are increasingly involved in delivering remote care, applying AI for predictive health analytics, and spearheading digital healthcare innovations. This evolution means we must reevaluate nursing education to include digital literacy, ensuring nurses are prepared for tomorrow's healthcare demands.
Trend Toward Personalized and Preventative Care
Healthcare is gradually shifting toward models that prioritize personalized and preventative care. Nurses, known for their patient-centered approach, are crucial in leading this shift. The demand for continuous professional development is paramount, enabling nurses to adapt to and advocate for advancements in patient care practices.
Policy Changes and Advocacy Efforts
There is a growing acknowledgment of the importance of supportive policies for nurses, emphasizing work-life balance, mental health, and professional development. Advocacy for enhanced compensation and better working conditions is gaining traction, promising to bolster nurse recruitment and retention efforts.
Collaborative Strategies for a Resilient Future
A collaborative effort among healthcare stakeholders is essential to adapt to these emerging trends. This involves crafting an adaptable, technologically proficient nursing environment committed to sustainable workforce development. Such collaborative efforts aim to ensure the nursing profession remains central to a resilient healthcare system capable of facing future healthcare challenges.
Building a More Resilient Nursing Workforce is Possible
This article outlined practical strategies for creating a resilient nursing workforce, emphasizing the importance of sustainable nurse staffing in healthcare environments. It focused on addressing the challenges of staffing shortages and high turnover rates that many institutions face today.
Investing in continuous education and providing support systems for nurses will ultimately build a more resilient nursing workforce. Implementing flexible scheduling and fostering a positive work culture are key steps toward achieving sustainable staffing levels and improving job satisfaction among nurses.
So, consider the strategies we outlined here as a foundation for change. Apply these insights to your institution, ensuring a healthier work environment for nurses and better patient care.