5 Unique Ways to Leverage PCU Nurses in Your Organization
Progressive Care Unit (PCU) nurses are critical assets to any healthcare organization. Their specialized skills and knowledge bridge the gap between intensive care and general medical-surgical care.
They also have advanced training in monitoring and managing complex health conditions. And that makes them versatile and invaluable.
Basically, leveraging progressive care nurses effectively can improve patient outcomes and streamline operations.
The point is to do it correctly.
This article explores 5 unique ways to integrate PCU nurses into your healthcare team. You can improve patient care, increase efficiency, and ensure better resource utilization by simply optimizing their roles.
Let’s dive into these innovative strategies to make the most of your PCU nursing staff.
What Is a PCU Nurse, And Why Do Facilities Need Them?
PCU is a specialty of nursing; PCU nurses are registered nurses (RNs) experienced in providing care to patients with complex medical conditions that require close monitoring and intervention but who are not critically ill enough to require the full resources of the ICU.
They are experts in managing patients who are medically fragile and at risk for instability. For a patient in a critical condition, these types of nurses can make all the difference.
The Value of PCU Nurses
PCU nurses bring significant value to healthcare organizations through their specialized skills and knowledge. They provide critical care to patients who are too ill for a general medical-surgical floor but do not need intensive care. In fact, more than 5 million patients are admitted annually to U.S. ICUs for intensive or invasive monitoring, support of airway, breathing, or circulation, and stabilization of acute or life-threatening medical problems.
PCU nurses increase your ROI: By effectively managing complex medical conditions, PCU nurses ensure high-quality patient outcomes and reduce hospital stays, which directly impacts your bottom line. Investing in the healthcare workforce, particularly nurses, has been shown to yield a return on investment at a ratio of 10:1.
PCU nurses are proficient in using advanced medical equipment and interpreting complex data. Their expertise enhances diagnostic accuracy and treatment efficacy, reducing errors and improving overall patient care quality. This proficiency contributes to a more efficient and effective healthcare environment. Moreover, PCU nurses excel in patient education and communication, playing a crucial role in helping patients understand their conditions and treatment plans. This empowerment leads to better compliance and health outcomes, enhancing patient satisfaction, which is critical for your reputation and patient retention.
Studies have shown that patient satisfaction affects clinical outcomes, patient retention, and medical malpractice claims. It affects the timely, efficient, and patient-centered delivery of quality health care. Furthermore, satisfied patients are more likely to return for future medical needs and post favorable comments and ratings online, directly influencing your organization's reputation.
PCU nurses are integral to quality improvement initiatives. They identify inefficiencies and suggest practical solutions based on their frontline experience. This proactive approach helps streamline processes and improve care delivery. Healthcare facilities can achieve a 3-5x return on investment through strategic retention methods that include competitive compensation, flexible scheduling, clear advancement paths, and ongoing professional development.
As you can see, you have a lot to gain from their insights into making your operations more cost-effective and patient-centered.
Nursing Trends and Landscape for 2025
Now more than ever, the medical industry and healthcare facilities are focusing on human and specialized care for all patients. Empathy, proactiveness, and quality care in PCU nursing are critical.
With new rising trends in the market, nurses in general are expected to excel in their roles. But what are these trends exactly, and how do they affect how nurses work?
Chronic Health Conditions and Illnesses
According to Davis & Elkins College, diabetes and hypertension are rising and require a specialized approach and care from nurses.
As this research points out:
“As chronic diseases rise, so too does the need for nurses trained to manage them.” - Davis & Elkins, Why the Nursing Field is Expected to Grow by 2025
The Pandemic´s Effect
The same analysis pointed out the effect that the pandemic had on the nursing profession, as it stated, “Suddenly, everyone knew how essential they were, working on the front lines.” This gave nurses a newfound respect, making the demand higher for patients with progressive care needs or just for a healthy patient recovery.
Nursing School
Nurse Registry has reported a small increase of 0.3% in enrollment in nursing; while this is still a win for the healthcare industry, it is not enough for the rising demand for nursing in a specialized department or PCU nurses.
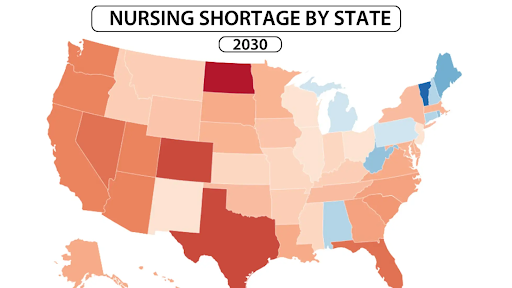
Because of this, a big shortage in nursing is projected by 2030 in the USA, especially in Texas and North Dakota. In fact, 91% of nurses believe that the nursing shortage is getting worse.
The Shortage in PCU
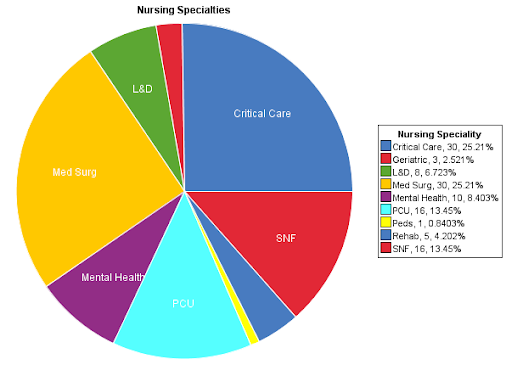
We know that work conditions, salary, and burnout are big parts of the nursing shortage and the main concern of the healthcare industry. If these weren't enough, of all nursing specialties, only 13.45% are PCU. This shortage only aggravates the problem and makes it even more difficult for medical facilities to find and retain PCU registered nurses.
Because of this shortage and lack of nursing staff, the recovery progress of many patients has been affected, and many terminal or critical patients do not get the proper assistance.
5 Ways to Better Leverage PCU Nurses
So, how can your healthcare facility leverage PCU nurses? How do you maximize the potential of this nursing specialty we find at a critical stage?
You can be part of the solution by providing a healthy workspace and thus leveraging the benefits of having PCU professionals in your organization.
1) Implement Specialized Training Programs to Enhance their Expertise in Critical Care
You need to enhance the capabilities of PCU nurses if you want to improve patient care quality and operational efficiency in your organization. Specialized training programs tailored to their unique roles can help them stay up to date with medical advancements and clinical practices.
How do you make sure you are providing the best-specialized program for your PCU nurses? There is a path to follow.
Start with a needs assessment by identifying specific skills and knowledge gaps among your PCU nurses. Use validated tools like the Hennessy-Hicks Training Needs Analysis (TNA) questionnaire to gather data through surveys, interviews, and performance reviews. Once you have a clear understanding of what’s missing, the next step is to develop a curriculum that addresses these gaps. Research shows that healthcare facilities with higher percentages of BSN nurses see better patient outcomes and lower mortality rates, emphasizing the value of advanced education in clinical skills, the latest technological tools, patient management techniques, and interdisciplinary communication.
To make the program truly effective, engage experts in the process. Bringing in experienced healthcare professionals and educators ensures that training modules are relevant and up to date. A study on blended learning reported a 100% attendance rate and a 97.75% satisfaction rate, highlighting the effectiveness of expert-led initiatives. But training doesn’t end with teaching—it must be continuously assessed. Use tools like the AACN Knowledge Assessment Tool to measure progress through theoretical and practical tests, ensuring that nurses gain the necessary competencies to handle PCU challenges.
Certification and incentives also play a crucial role in motivation. Providing career advancement opportunities and financial bonuses upon successful completion of training has been shown to significantly improve nurse retention and job satisfaction, leading to better patient care.
Finally, monitor outcomes to ensure that the investment in nurse training is delivering tangible results. Tracking patient care improvements and operational efficiency provides valuable data to demonstrate program impact. A study on training effectiveness found that nurses’ communication knowledge scores increased significantly, proving that well-structured training programs translate into better patient outcomes.
Specialized Knowledge from Conferences
Conferences are the perfect way to leverage and grow the knowledge of your PCU nurses. These are some of the most awaited informational conferences this year in the nursing space.
2) Use PCU Nurses for Cross-Functional Roles in Different Departments
Integrating PCU nurses into cross-functional roles can enhance team dynamics, improve patient care, and optimize resource utilization. Basically, you’ll leverage their specialized skills across various departments, providing a well-rounded and adaptable workforce.
Here’s how you can implement this strategy in your organization:
Identify Key Departments: Determine which departments would most benefit from the expertise of PCU nurses. Consider areas like the intensive care units (ICU), emergency department, and outpatient services.
Assess Skill Sets: Evaluate your PCU nurses' specific skills and experiences. Match these competencies with the needs of the identified departments.
Develop Cross-Training Programs: Create comprehensive training programs to equip PCU nurses with the necessary skills for their new roles. Include department-specific protocols, procedures, and tools.
Implement Rotational Schedules: Establish rotational schedules that allow PCU nurses to work in different departments. Ensure these rotations are frequent enough to maintain familiarity but not so frequent that they cause disruption. There are plenty of nurse scheduling software that would help you here.
Provide Ongoing Support: Offer continuous support and resources as nurses transition into their cross-functional roles. Include mentorship programs and access to additional training materials.
Evaluate Outcomes: Regularly review the outcomes of this cross-functional approach. Assess improvements in patient care, resource efficiency, and staff satisfaction.
How To Assess Skill Sets
We advise conducting a quarterly review of cross-functional deployments to identify best practices and areas for improvement by assessing the skill sets of new and old employees.
To accurately conduct an assessment, first, you need to understand the skill you want to assess. In the PCU field, this might be soft skills like empathy and comprehension of elderly patients.
Later, you can choose from different assessment methods, like Psychometric tests, personality tests, or even mental ability assessments. These are perfect for assessing soft skills.
Conduct an implementation plan to implement your desired assessment before analyzing the results and providing feedback to your nurses.
3) Engage Nurses in Telehealth Initiatives for Remote Patient Monitoring
Basic procedures like taking vital signs or administering injections can be performed by trained personnel with the real-time remote guidance of a nurse. However, direct supervision is still necessary to ensure patient safety and proper technique.
Their role extends beyond procedural guidance, including virtual patient education, medication management, post-discharge follow-ups, chronic disease monitoring, and telehealth consultations. By leveraging remote nursing, healthcare facilities can improve patient access to care, reduce hospital readmissions, and enhance overall efficiency.
This gives your facility an advantage, making it easy for at-home patients and allowing you to keep your PCU at the actual facility, reducing translation and even equipment costs.
According to recent stats, approximately 25% of nurses spend a significant portion of their time in telehealth roles. This means that the other percentage of the time can be spent in hospitals and clinics with other patients.
Leveraging PCU nurses in telehealth initiatives leads to better patient monitoring and care delivery. Their expertise and adaptability make them ideal candidates for managing remote patient interactions. And that ensures continuity of direct care.
Here's how to integrate PCU nurses into your telehealth programs:
Evaluate Telehealth Needs: Identify the specific telehealth services that would benefit from the inclusion of PCU nurses. Consider chronic disease management, post-discharge follow-ups, and patient education.
Equip with Technology: Provide PCU nurses with the necessary telehealth tools and platforms and ensure they are trained to use these technologies effectively to conduct virtual consultations.
Develop Protocols: Establish clear protocols for telehealth interactions. Define the scope of practice, patient triage processes, and escalation procedures for virtual care.
Training and Certification: Offer specialized training in telehealth best practices. Include certification programs to validate their proficiency in remote patient care.
Integrate with EHR Systems: Ensure telehealth platforms are seamlessly integrated with your electronic health record (EHR) systems. This integration allows for efficient documentation and access to patient histories during virtual visits. If it helps, partnering with AllScripts EHR Implementation / Optimization Consultants ensure seamless integration of electronic health record.
Patient Education: Train PCU nurses to educate patients on using telehealth services. Provide resources and support to help patients become comfortable with remote consultations.
Quality Assurance: Implement a quality assurance program to monitor telehealth interactions. Regularly review recorded sessions and patient feedback to maintain high standards of care.
Monthly Virtual Telehealth Debrief Sessions
We suggest scheduling monthly virtual telehealth debrief sessions for those in-house and remote nurses. These sessions allow PCU nurses to share experiences, discuss challenges, and suggest improvements.
This collaborative approach ensures continuous enhancement of your telehealth services, leading to better patient outcomes.
Make sure to have a virtual lead; this could be a manager or someone who is specifically there to guide the meeting in the right way. Learn how to run a virtual telehealth session.
4) Assign Nurses to Lead Patient Education and Support Groups
Empowering Progressive Care Unit (PCU) nurses to lead patient education and support groups can significantly enhance patient outcomes and satisfaction. Studies have shown that patients who receive structured education from qualified nurses exhibit improved self-care behaviors and increased disease knowledge, with effects persisting for at least six months.
To implement this strategy, begin by assessing the specific educational needs of your patient population, focusing on areas such as chronic conditions, post-operative care, and lifestyle modifications. It's noteworthy that 94% of patients desire educational materials from their healthcare providers, yet only about two-thirds report receiving them, highlighting a significant opportunity to address unmet educational needs.
Next, develop a structured curriculum for each support group that includes evidence-based information, practical tips, and interactive elements to engage patients. Research indicates that patients can forget between 40% to 80% of medical information provided during consultations, emphasizing the importance of well-structured and memorable educational content.
Select PCU nurses with strong communication skills and a passion for patient education, providing additional training to enhance their facilitation abilities. Enhanced nursing education has been linked to improved patient outcomes, including decreased mortality rates and shorter hospital stays.
Organize regular group sessions to ensure continuity and build a supportive community, offering both in-person and virtual options to accommodate patient preferences. Regular engagement has been shown to improve patient activation levels, leading to better health behaviors and outcomes.
Develop comprehensive educational materials such as pamphlets, videos, and online resources, ensuring these materials are accessible and easy to understand. Given that only about 50% of hospitalized patients have adequate health literacy, it's crucial to create materials that cater to varying literacy levels.
Incorporate interactive activities like Q&A sessions, demonstrations, and group discussions to help patients absorb information and apply it to their daily lives. Interactive education methods have been associated with better patient engagement and adherence to treatment plans, ultimately leading to improved health outcomes.
The Buddy System Program
We recommend implementing a buddy system within the support groups. Pairing new members with experienced ones can enhance the learning experience and foster a sense of community.
By implementing checklists, paring the right peers, setting expectations, and doing regular check-ins, your buddy program is on the path to success.
This approach boosts patient confidence and improves adherence to care plans.
5) Involve Nurses in Clinical Research and Quality Improvement Projects
Engaging PCU nurses in clinical research and quality improvement projects drives innovation and elevates care standards within your organization. Their firsthand experience with patient care positions them uniquely to identify improvement opportunities and contribute significantly to research initiatives.
To effectively involve PCU nurses in these endeavors, begin by identifying their specific areas of interest and expertise. Aligning these interests with organizational goals and patient needs ensures that projects are both relevant and impactful. Studies have shown that nurses with positive attitudes toward research are more likely to utilize evidence-based practices, leading to improved patient outcomes.
Next, offer specialized training in research methodologies, data analysis, and ethical considerations. Equipping nurses with these skills enables them to conduct rigorous and ethical research. For instance, nurse-led research has been instrumental in developing interventions that reduce patient readmissions and enhance care quality.
Form multidisciplinary research teams that include PCU nurses, physicians, and other healthcare professionals. This collaborative approach enriches the scope of research projects, fostering innovation. A notable example is the development of the Symptom Distress Scale by nurses, which has become a pivotal tool in assessing patient discomfort.
Define clear, measurable objectives for each research or quality improvement project. Ensuring that all team members understand the goals and their roles in achieving them is crucial for success. Evidence suggests that well-structured nurse-led initiatives can lead to significant improvements in patient care processes.
Allocate necessary resources, such as funding, time, and access to data. Organizational support is vital for the success of these initiatives. Investing in nurse-led research has been shown to advance the scientific practice of nursing and improve patient outcomes.
Encourage a culture of innovation where nurses feel empowered to propose new ideas and approaches. Regular brainstorming sessions can generate novel solutions, leading to advancements in patient care. For example, nurse-led solutions have been pivotal in addressing challenges such as workplace violence and emergency care delivery.
Implement pilot programs to test new ideas before full-scale implementation. This approach allows for adjustments based on initial results and feedback, ensuring the effectiveness of new interventions. Nurse-led action research projects have successfully expanded roles in patient education, leading to greater professional accountability.
Finally, continuously monitor and evaluate the progress of research projects and quality improvement initiatives. Using established metrics to assess outcomes facilitates data-driven decisions, ultimately enhancing patient care. Engaging bedside nurses in research and quality improvement has been linked to increased utilization of evidence-based practices.
Quality Improvement Committee
Establish a dedicated research and quality improvement committee. This committee, including PCU nurses, can oversee projects, provide guidance, and facilitate access to necessary resources.
This structured support enhances the likelihood of successful outcomes and sustained improvements in care quality.
Leverage Your PCU Nurses Effectively
As you can see, leveraging PCU nurses effectively can transform your healthcare organization. Their expertise bridges critical care and general medical care. Ultimately, this allows you to enhance patient outcomes.
Besides, using their skills in patient education can improve health literacy and outcomes. And engaging them in leadership roles fosters innovation and best practices.
Additionally, their ability to manage complex cases ensures efficient resource use.
So, implement these 5 strategies above to elevate your healthcare delivery and operational efficiency.
Contact us today to streamline your PCU and medical staffing solutions and organizational success.
FAQs
What do PCU nurses do?
PCU nurses provide direct care to patients with complex medical needs who require close monitoring and intervention but who are not critically ill enough to require the full resources of the ICU. They manage patients with a wide range of conditions, including any cardiac conditions or issues, respiratory problems, neurological conditions, and post-operative needs.
What does PCU stand for?
PCU stands for Progressive Care Unit. It is also sometimes referred to as a step-down unit, intermediate care unit, or telemetry unit.
Where do PCU nurses work?
PCU nurses work in hospitals, specifically within the Progressive Care Unit. This unit is a designated area within the hospital designed to provide care for patients who require a higher level of monitoring and care than is available on the general medical-surgical floor but not the intensive care of the ICU.
What is a Telehealth nurse?
A Telehealth nurse provides healthcare services remotely using technology, such as video conferencing and phone calls. They assess patients, provide education, monitor chronic conditions, and offer support, all from a distance. A Telehealth nurse's primary mode of patient interaction is virtual, whereas a PCU nurse works directly with patients in a hospital setting.
What are the additional requirements of PCU nurses?
PCU nurses typically have several years of experience as registered nurses (RN) and often hold certifications in critical care nursing or other relevant specialties. They require advanced clinical skills, strong assessment abilities, and the ability to work effectively under pressure. Excellent communication and teamwork skills are also essential.
Can a PACU nurse do ICU?
Yes, with additional training. PACU and ICU share critical care skills, but ICU requires experience in prolonged intensive monitoring.
How many patients should a PCU nurse have?
Typically, 3-5 patients per nurse, depending on acuity levels and hospital staffing ratios. Lower ratios improve patient safety and care quality.